Pregnancy and Kidney Stones
What You Should Know About Kidney Stones During Pregnancy
Kidney stones are a fairly common urological problem, affecting about 1 in 10 people at some point in their life. But kidney stones can be a particular challenge for pregnant women. The way stones are diagnosed and treated may need to be adjusted during pregnancy for the safety of the mother and her baby.
Still, pregnant women with kidney stones have several treatment options. And it’s important to know that without treatment, kidney stones can lead to premature labor, so it’s necessary to address them.

What are kidney stones?
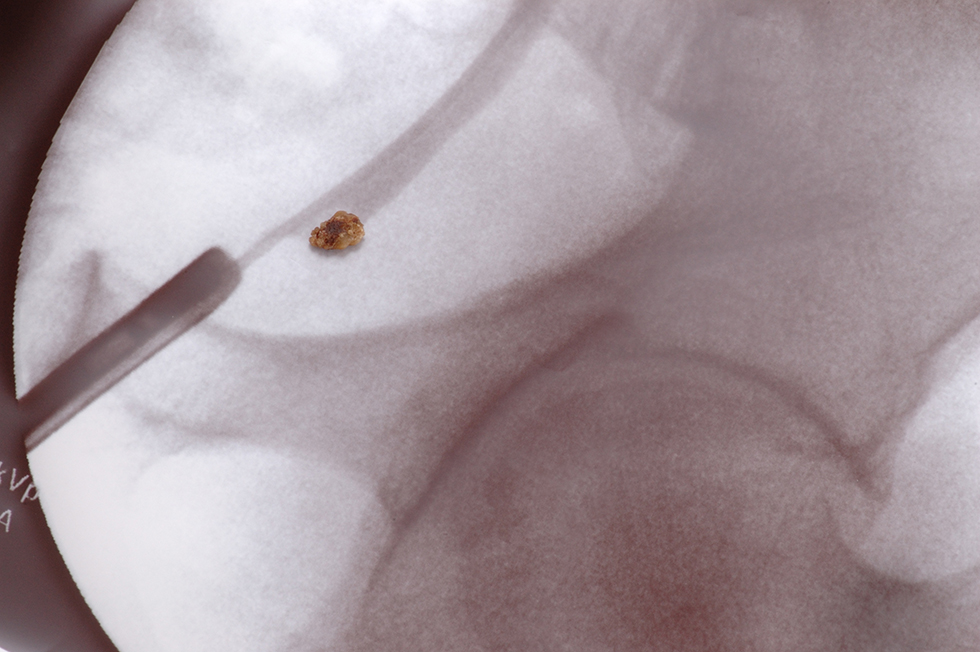
Kidney stones are small, crystallized masses that form in the kidneys or ureters (the tubes connecting the kidneys to the bladder). Most stones are made from calcium, but they can also be formed from uric acid, struvite, and cystine, which are naturally occurring compounds in the human body. Kidney stones come in various shapes and sizes and can be smooth or jagged, small as a pea, or as large as a golf ball.
Most kidney stones are small enough to pass through the urinary tract on their own. A person with a small kidney stone might not have any symptoms.
But larger stones can block urine flow and cause a significant amount of pain. In fact, abdominal pain is one of the most common symptoms of kidney stones. Some people have nausea and vomiting, along with a need to urinate more urgently and frequently. Blood in the urine is another symptom.
How common are kidney stones in pregnant women?
It’s estimated that kidney stones occur in about 1 of every 500 to 3,000 pregnancies, so having kidney stones during pregnancy is fairly rare.
However, research suggests that risk for first-time kidney stone formation is higher at certain points in a pregnancy.
In 2021, the American Journal of Kidney Diseases published a study on the topic. Researchers found that in pregnant women, risk for developing first-time symptomatic kidney stones increased during the second and third trimesters of pregnancy.
Interestingly, the peak time to develop kidney stones was during the first 3 months after delivery. About a year after the delivery date, risk returned to pre-pregnancy levels.
Risk was higher in pregnant women who were obese.
Why are pregnant women more at risk for kidney stones?
Pregnant women are more prone to kidney stones for the following reasons:
- Pregnant women are more susceptible to dehydration. A growing baby puts pressure on a woman’s bladder, increasing the need to urinate. As a result, pregnant women might not drink as much fluid as they should, and dehydration can lead to kidney stones.
- Changes occur in urine composition during pregnancy. Pregnant people tend to have more calcium in their urine, and most kidney stones are calcium-based.
- Hormonal changes in pregnant women make it more difficult to clear urine from the body. Pregnant women have higher levels of the hormone progesterone, which contributes to urinary stasis (halting of or slowing of urine flow). As a result, stone-forming compounds have more opportunity to crystallize.
How are kidney stones diagnosed in pregnant women?
Diagnosis starts with a medical history. Designing a personalized treatment plan requires knowing more about your symptoms, your pregnancy, and your medical background.
Lab tests are also an important diagnostic tool. These include blood tests and urine tests. Urine tests may reveal if stone-forming substances are present.
Imaging tests may also be ordered. These tests can reveal the location, size, and shape of any kidney stones:
- Ultrasound. Ultrasound technology uses sound waves to create images of internal organs. (It’s also used to monitor the development of a baby in the uterus.) No radiation is used with ultrasounds, so they are perfectly safe for both the patient and the fetus. For a kidney stones diagnosis, ultrasound technicians focus on the kidney and pelvic area.
- Magnetic resonance (MR) urography. Urography refers to imaging of the urinary tract: kidneys, ureters, bladder, and urethra. Magnetic resonance (MR) technology creates images using magnet and radio waves. Like ultrasound technology, MR does not use radiation.
- Low-dose computed tomography (CT scan). A CT scan (sometimes called a “cat scan”) uses x-rays to create images. Because this method does involve radiation, it is recommended for the second and third trimesters only, not the first trimester.
How are kidney stones treated in pregnant women?
Kidney stone treatment in pregnant women requires a team approach. Urologists work with obstetricians and other healthcare specialists to make sure treatment is safe and appropriate.
Initial therapies may include the following:
- Observation. Generally, treatment starts with observation, a “wait and see” approach, as most stones pass on their own. Some doctors recommend bed rest, increased fluid intake, and a low-salt diet.
- Pain relief. Patients might be given pain relievers, such as acetaminophen. Other medications, such as non-steroidal anti-inflammatory drugs (NSAIDS) might be prescribed depending on the stage of the pregnancy. Patients should take their medication exactly as prescribed.
- Hydration. Patients may be advised to drink more fluids. Others may receive hydration via intravenous (IV) fluids at the doctor’s office to help stones pass.
If stones do not pass easily, procedures to extract stones or effect passage of urine around stones are considered. If symptoms are not severe, such procedures might be delayed until after the baby is born. In the case of more serious symptoms, trouble urinating, or a urinary tract infection, the patient may undergo treatment during the pregnancy. (In emergencies, these procedures might take place right away.)
The treatment team will carefully consider choices related to any anesthesia and related drugs given during these procedures.
Procedures to extract stones or effect passage of urine around stones include the following:
- Ureteroscopy. Patients undergoing ureteroscopy receive anesthesia. Once it has taken effect, the urologist places a long, thin instrument called a ureteroscope through the urethra and bladder to the ureter or kidney. The ureteroscope is like a tiny telescope that allows the doctor to see into the affected area. The ureteroscope also has a grasping mechanism that allows it to either remove the stone or break it into smaller stones that can pass through urine.
- Stent. A stent is a plastic tube that is surgically placed in the ureter to keep it open. With a stent, urine—and the stone—may flow through the ureter more easily. Stents are temporary; in pregnant patients, they are usually replaced every 4 to 6 weeks.
- Nephrostomy tube. A nephrostomy tube is a type of catheter used to drain urine from the kidney. Typically, urine flows from a kidney to the bladder through a ureter that connects these two organs. With a nephrostomy tube, urine bypasses the ureter and bladder. The surgeon creates a special opening called a stoma on the patient’s side. The nephrostomy tube runs from the kidney and through the stoma, connecting to a urine collection bag outside the body.
Like stents, nephrostomy tubes are temporary and may need to be changed periodically. Patients receive thorough instructions on the care of their tube and the changing of their urine collection bag.
Resources
American Academy of Family Physicians
“Magnetic Resonance Imaging (MRI)”
(Last updated: June 23, 2020)
https://familydoctor.org/magnetic-resonance-imaging-mri/
American Journal of Kidney Diseases
Thongprayoon, Charat, et al.
“Risk of Symptomatic Kidney Stones During and After Pregnancy”
(Published: April 15, 2021)
https://www.ajkd.org/article/S0272-6386(21)00402-9/fulltext
American Urological Association
Assimos, Dean, et al.
“Surgical Management of Stones: AUA/Endourology Society Guideline (2016)”
(Published: 2016)
https://www.auanet.org/guidelines/guidelines/kidney-stones-surgical-management-guideline
Healthline.com
Seladi-Schulman, Jill, PhD
“Caring for Your Nephrostomy Tube”
(Update: September 18, 2018)
https://www.healthline.com/health/nephrostomy-tube-care
MedlinePlus.gov
“CT Scans”
(Page last updated: April 12, 2021)
https://medlineplus.gov/ctscans.html
“Ultrasound”
(Page last reviewed: December 15, 2020)
https://medlineplus.gov/lab-tests/sonogram/
Medscape
Harrison, Pam
“Pregnancy Increases Risk for Symptomatic Kidney Stone”
(April 28, 2021)
https://www.medscape.com/viewarticle/950073
Nature Reviews | Urology
Semins, Michelle J. and Brian R. Matlaga
“Kidney stones during pregnancy”
(Published online: February 11, 2014)https://www.nature.com/articles/nrurol.2014.17″ https://www.nature.com/articles/nrurol.2014.17
Accessed via: https://svmi.web.ve/wh/intertips/7.UROLITIASIS-Y-EMBARAZO.pdf” https://svmi.web.ve/wh/intertips/7.UROLITIASIS-Y-EMBARAZO.pdf
NEJM Journal Watch
O’Dwyer, Marie Claire, MB BCh BAO, MPH
“Are Pregnant people More Likely to Develop Kidney Stones?”
(September 22, 2021)
https://www.jwatch.org/na54060/2021/09/22/are-pregnant-women-more-likely-develop-kidney-stones
UpToDate
Preminger, Glenn M., MD and Gary C. Curhan, MD, ScD
“Kidney stones in adults: Kidney stones during pregnancy”
(Topic last updated: November 11, 2021)
https://www.uptodate.com/contents/kidney-stones-in-adults-kidney-stones-during-pregnancy
Urology Care Foundation
“Pregnancy and Kidney Stones”
(Summer 2019)
https://www.urologyhealth.org/healthy-living/urologyhealth-extra/magazine-archives/summer-2019/did-you-know-pregnancy-and-kidney-stones
“Preventing and Treating Kidney Stones”
(Summer 2014)
https://www.urologyhealth.org/healthy-living/urologyhealth-extra/magazine-archives/summer-2014/preventing-and-treating-kidney-stones
Urology Marketing Center
“Kidney Stones”
https://www.hsadeghi.com/patient-education/kidney-stones/