What are kidney stones? How do they form?
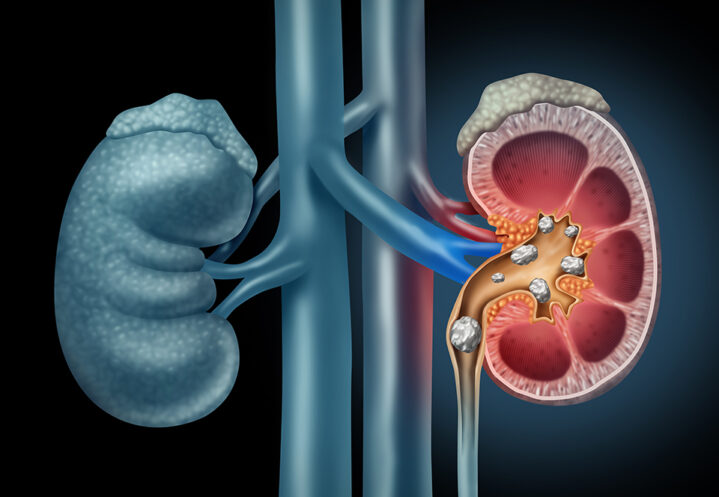
A kidney stone is a small mass that forms from crystallized substances in your kidney or, in some cases, one of your ureters (the tubes that connect the kidneys to the bladder). These chemicals aren’t able to dissolve in urine, so the crystals stick together and get larger, forming the stone. (Note: Stones that form in the ureters are called ureteral stones.)

You can be especially prone to kidney stones if you’re frequently dehydrated and there is less water to dissolve the substances. You can also develop them if your levels of the chemicals that crystallize to form stones are too high.
Kidney stones vary in size, shape, and color.
They are also made from different substances, depending on the type of stone.
Most stones are less than 5 mm in diameter (about 3/16 of an inch) and they usually pass on their own through urine. But sometimes, stones become larger or have trouble passing through the urinary tract. If this happens, you’ll need treatment, which we’ll discuss below.
Other terms for kidney stones are renal stone disease, nephrolithiasis and urolithiasis. Why are there so many names for kidney stones? The other names are scientific names. Both the word “renal” and the prefix “nephro” mean “relating to the kidneys” and scientists may sometimes refer to kidney stones as renal calculi or nephroliths.
Who gets kidney stones?
The National Kidney Foundation estimates that one in ten people will get a kidney stone at some point in their lifetime and that each year, about half a million people go to the emergency room because of kidney stones.
Men tend to get kidney stones more often than women do. Stones are most common in people over age 30.
Men tend to get kidney stones more often than women do. Stones are most common in people over age 30.
What Causes Kidney Stones?
Kidney stones form from substances found in your urine, like uric acid, calcium, oxalate, and cystine. You can get kidney stones if you have high levels of these substances in your system. But you might also get them if your body doesn’t make enough urine.
In either case, tiny crystals form and gradually get bigger, making a stone. Most of the time, stones just travel through your urinary tract and pass with your urine. But sometimes, they get stuck on the way and block urine flow. (If a stone gets stuck in your ureter, it’s called a ureteral stone.)
What are the Risk Factors for Kidney Stones?

Here are some common risk factors for kidney stones:
Your family history. If you have an immediate family member – a parent, brother or sister – with a history of kidney stones, you’ll be more likely to develop them yourself.
Dehydration. When you become dehydrated, your body doesn’t produce as much urine and stone-forming substances have a harder time dissolving.
Bowel problems. Frequent diarrhea can make you dehydrated.
Your diet. High levels of calcium, salt, and animal protein can make you more susceptible to kidney stones. It’s possible that you’re consuming too much of these items in your diet. But it’s also possible that your body isn’t processing them as it should. Once we know more about your kidney stones, we can advise you on foods to choose and foods to avoid.
Health conditions. Obesity, abnormal growth of parathyroid glands (glands that produce a hormone that regulates levels of calcium and phosphorus in the body), and distal renal tubular acidosis (excess amounts of acid in the blood as a result of poor kidney function) are kidney stone risk factors.
Medications and supplements. For example, if you take calcium or vitamin C supplements, you might be more prone to kidney stones. If you make a list of the medications and supplements you take, we can review it with you.
How are kidney stones classified?
Kidney stones vary in size, shape, and color. They are also made from different substances, depending on the type of stone. Knowing of the type of kidney stone you have helps us treat it most effectively.
Calcium stones. Most kidney stones (about 80%) are made from either calcium oxalate or calcium phosphate. These can form if there’s too much calcium in your urine.
Uric acid stones. Uric acid is produced when your body breaks down compounds called purines, which are found in foods like anchovies, dried beans, and peas. When uric acid crystals accumulate, they can form a uric acid stone.
Struvite stones. Struvite stones are more common in people who get frequent urinary tract infections (UTIs). Bacteria that cause UTIs disrupt the chemical balance in the urine. Struvite stones are sometimes called staghorns because they have a jagged appearance.
Cystine stones. This type of stone, made from an amino acid called cystine, is caused by a rare inherited condition called cystinuria. People with cystinuria have too much cystine in their urine.
Symptoms
Symptoms may be different depending on the type of stone you have, but some of the more typical symptoms are:
You might have heard stories about pain associated with kidney stones because the pain can be intense, but it’s not always so.
Pain
You might have heard stories about pain associated with kidney stones because the pain can be intense, but it’s not always so. Usually pain occurs when urine can’t flow past the stone. You might feel pain in your back, side, abdomen, or groin. Pain can be mild, but it can also be severe. Periods of severe pain are called renal colic.
We can help you manage the pain, but if it becomes unbearable and you are unable to reach us, don’t hesitate to head to the ER.
Some men feel pain in their testes or penis as the stone passes. Once the stone is passed, the pain stops.”
Blood in your urine (hematuria) or “sand.”
If you have blood in your urine, you might see a pink or reddish tint in the toilet. But it’s also possible that you won’t see anything different at all. Microscopic hematuria occurs when the blood particles are too small to see with the naked eye.
You might also notice tiny stones in your urine. Urologists call the particles “gravel” or “sand.”
Urination changes
You might urinate more frequently or feel like you need to go to the bathroom more often, even if you don’t produce much or any urine. You could also have pain or a burning sensation when you urinate.
Nausea. You might start vomiting.
It’s also possible for people with kidney stones to have no symptoms at all.
Diagnosing Kidney Stones
When you come see us, we’ll start by taking a complete medical history. Be sure to tell us about your diet. That can give us some important clues. We’ll also ask about the medications you take and whether anyone in your family has had stones before.
Next, we’ll do some blood and urine tests. Substances that form stones, like calcium and uric acid, may be present in your urine. Imaging tests, such as a CT scan (a “cat” scan – computed tomography) or an ultrasound, are also likely. These tests can indicate the size, shape, and quantity of kidney stones.
Your symptoms, medical history, and test results will tell us how to treat your kidney stones.
Kidney Stone Treatment
If your stone is small and your pain is mild, you might be able to manage your kidney stone at home. If it’s safe for you, we’ll recommend nonsteroidal anti-inflammatory drugs (NSAIDS) like ibuprofen or naproxen. We might also prescribe medication like tamsulosin, which can help your stone pass by relaxing the ureter. This process can take a few weeks.
We might ask you to strain your urine when you’re home. If you catch the stone as it passes, save it and bring it to us for analysis. This will help us determine what type of stone it is.
If your stone is large or doesn’t pass on its own after 4 to 6 weeks, you’ll need more advanced treatment. You will likely have imaging tests and a urinalysis beforehand. These tests results help us choose the best treatment for you.
Ureteroscopy
This procedure is generally used to treat stones in your kidney or ureter. We will use a thin instrument called a ureteroscope to get a better view of the stone. The ureteroscope can also remove the stone or break it into smaller pieces that can pass on their own. After you have received anesthesia, we will thread the ureteroscope through your urethra and bladder until it reaches the ureter or kidney.
Chances are, you’ll be able to go home the same day as your ureteroscopy and go back to your daily routine in two to three days.
After a ureteroscopy, we might insert a temporary stent – a small tubelike structure – in your ureter to keep it open. This is usually removed about four to ten days after your procedure.
Shock wave lithotripsy (SWL)
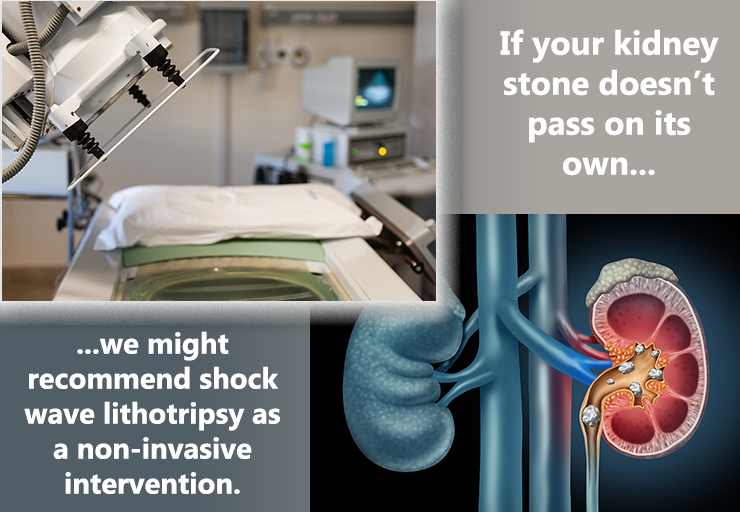
SWL uses shock waves that go through your skin, hit the stone’s surface, and break it into smaller pieces that can pass more easily. You will likely receive anesthesia. Many patients go home the same day as their procedure and can resume their normal activities in two or three days. Afterward, you might see blood in your urine, and you could still have some discomfort while the remaining kidney stone fragments pass. We might prescribe medication to help them pass.
SWL isn’t recommended for people with large or hard stones.
Percutaneous nephrolithotomy (PNL)
PNL can be helpful for people with larger kidney stones. You will be anesthetized for the procedure. We will start by making a small incision in your back or side. This incision allows us to examine your kidney with a tool called a nephroscope. Another instrument, which can break stones and remove them with suction, is passed through the nephroscope.
After the procedure, we might leave a tube in your kidney (called a nephrostomy tube) for a day or two to allow urine to pass into a bag outside your body. You might also have a temporary stent.
In addition, we might order x-rays to make sure there are no residual kidney stones left. If any stones are found, they can be removed while you are still in the hospital.
Depending on the extent of your treatment, you might be in the hospital for a few days for PNL. You should be able to return to your usual activities in a week or two.
Which procedure is best?
As mentioned above, the answer depends on your situation. For example, shock wave lithotripsy has low complication rates, but ureteroscopy could address all the stones with one procedure.
Patients who don’t have success with the approaches mentioned above may need to have laparoscopic, open, or robot assisted surgery to remove the stone.
What are stents?
Your treatment might include a ureteral stent, especially if a stone is blocking one of your ureters. A stent is a plastic tube that keeps the ureter open so that urine can flow around the stone. A stent may also be used after surgical procedures so that the ureter can heal.
Some people need stents for just a couple of days. For others, the time frame might be longer. If your stent is uncomfortable, we can prescribe medication.
Kidney Stones Without Symptoms
As we mentioned earlier, not all stones have symptoms. You might not even realize you have a stone until you have an imaging test for another health issue. In these circumstances, stones might not need treatment. However, we might recommend having asymptomatic stones removed if we think they will grow and cause discomfort later. You’ll need to think about how quickly you could get treatment if the stone started giving you trouble.
Preventing Future Kidney Stones
Once you’ve had a kidney stone, you’re at higher risk for having another one. During your follow-up appointments, we’ll monitor your situation and conduct urine, blood, and imaging tests as needed. We’ll also analyze your original kidney stone(s) if we can. Knowing what they’re made of can help us develop a plan going forward.
There are also steps you can take to lower your risk for another stone. We’ll provide specific instructions tailored to your situation. But some of the most common prevention strategies include the following:
Drink more fluids

Experts recommend drinking about 10 servings of 10 fluid ounces each day. (Some experts say 3 quarts or 3 liters.) This will increase the amount of urine that your kidneys process and help substances dissolve so they won’t form crystals in the future.
Water is ideal, but other beverages, like tea and coffee, “count” toward your fluid intake. It’s not a bad idea to keep a checklist of the amount of fluid you’ve had each day. It also helps to use bottles and cans that list fluid measurements on the label.
Change your diet
We’ll go over your diet with you thoroughly. You might need to eliminate or cut down on salty foods, like cheese, deli meats, and certain snacks. You might need to reduce your calcium intake or eat foods that are low in oxalate. Or, we might recommend eating less animal protein (meat, fish, poultry, etc.).
Take medications as directed. Depending on your situation, we might prescribe drugs like
- thiazide diuretics – a type of drug that increases urine flow
- Allopurinol – a drug that decreases uric acid production
- potassium citrate – a drug that makes urine less acidic
- acetohydroxamic acid – medication used to treat bladder infections, which can cause struvite stones
- or cystine-binding thiol drugs- medications used to dissolve cystine stones
We will explain any medication’s purpose and be sure you understand how and when to take it.
Pay attention to your urologic health
If you notice anything unusual – pain with urination, for example – give us a call. We’ll be watching for urinary tract infections (UTIs) and other conditions that may affect your urologic health.
Resources
American Family Physician
“Preventing Kidney Stones with Diet and Nutrition”
(December 1, 2011)
https://www.aafp.org/afp/2011/1201/p1243.html
American Urological Association
“Medical Management of Kidney Stones (2019)”
(Published 2014. Reviewed and validity confirmed 2019)
https://www.auanet.org/guidelines/kidney-stones-medical-mangement-guideline#x2864
“Surgical Management of Stones: AUA/Endourology Society Guideline (2016)”
(Published 2016)
https://www.auanet.org/guidelines/kidney-stones-surgical-management-guideline
Healthline.com
Roland, James
“Hard Water vs. Soft Water: Which One Is Healthier?”
(July 30, 2019)
https://www.healthline.com/health/hard-water-and-soft-water
Watson, Stephanie
“Struvite: The Less Common Type of Kidney Stone”
(March 12, 2018)
https://www.healthline.com/health/kidney-health/struvite-stones
MedlinePlus.gov
“Allopurinol”
(Page last updated: August 15, 2017)
https://medlineplus.gov/druginfo/meds/a682673.html
“Parathyroid Disorders”
(Page last updated: October 21, 2020)
https://medlineplus.gov/parathyroiddisorders.html
“Uric acid – blood”
(Page last updated: October 8, 2020)
https://medlineplus.gov/ency/article/003476.htm
Medscape
Biyani, Chandra Shekhar, MS, MBBS, DUrol, FRCS(Urol), FEBU
“Cystinuria Treatment & Management”
(December 12, 2019)
https://emedicine.medscape.com/article/435678-treatment#d6
National Kidney Foundation
“How common are kidney stones?”
(Date reviewed: June 7, 2020)
https://www.kidney.org/atoz/content/kidneystones
“NKF Answers Top 10 Questions about Kidney Stones”
https://www.kidney.org/news/ekidney/november10/Top10_November10
“Distal Renal Tubular Acidosis (dRTA): What is dRTA and how is it diagnosed?”
(Reviewed: June 7, 2019)
https://www.kidney.org/atoz/content/distal-renal-tubular-acidosis-drta-what-drta-and-how-it-diagnosed
“What are Cystine Stones?”
(Last reviewed: March 8, 2016)
https://www.kidney.org/atoz/content/what-are-cystine-stones
UpToDate.com
Preminger, Glenn M., MD and Gary C. Curhan, MD, ScD
“Patient education: Kidney stones in adults (Beyond the Basics)”
(Last updated: October 10, 2019)
https://www.uptodate.com/contents/kidney-stones-in-adults-beyond-the-basics
Urology Care Foundation
“Did You Know? Ureteral Stents”
(Summer 2020)
https://urologyhealth.org/healthy-living/urologyhealth-extra/magazine-archives/summer-2020/did-you-know-ureteral-stents
“What are Kidney Stones?”
(Updated: April 2020)
https://www.urologyhealth.org/urologic-conditions/kidney-stones
WebMD
“Acetohydroxamic Acid Tablet”
https://www.webmd.com/drugs/2/drug-8724/acetohydroxamic-acid-oral/details