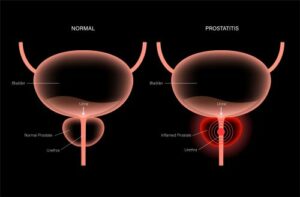
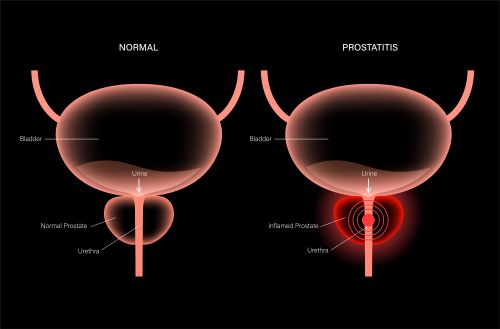
Prostatitis—inflammation of the prostate gland—is a painful condition that can make urination and sexual intercourse difficult. Experts estimate that between 35% and 50% of men develop prostatitis symptoms at some point in their lives. It can happen to men of all ages.
The prostate is a small, walnut-shaped gland located between the penis and the bladder. Part of the urethra (the tube from which urine and semen exit the penis) is surrounded by prostate tissue.
35% ~ 50% of men develop prostatitis symptoms at some point in their lives
The prostate is an important gland for male reproduction. It contracts when a man ejaculates, closing off the pathway between the bladder and urethra so that urine doesn’t mix with semen. It also produces prostatic fluid, which nourishes sperm cells and helps them travel toward an egg after ejaculation.
Types of Prostatitis
Urologists classify prostatitis into 4 types:
- Acute bacterial prostatitis. Caused by bacteria, this type of prostatitis comes on suddenly, and symptoms can be severe. But with proper treatment, it goes away fairly quickly.
- Chronic bacterial prostatitis. This type is also caused by bacteria, but symptoms start gradually and tend to be less severe. However, they usually last longer. Men with chronic bacterial prostatitis may have symptoms for several months.
- Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). This is the most common type of prostatitis. It’s not caused by bacteria. In fact, scientists aren’t exactly sure what causes it, but research is ongoing.
- Asymptomatic inflammatory prostatitis. When an illness is asymptomatic, it doesn’t cause any symptoms. Men might not be aware they have this type of prostatitis. It is often discovered during tests for other urologic conditions. It does not have complications and doesn’t require treatment.
Because asymptomatic inflammatory prostatitis does not need treatment, this article will focus on acute bacterial prostatitis, chronic bacterial prostatitis, and CP/CPPS.
Bacterial Prostatitis
What causes bacterial prostatitis?
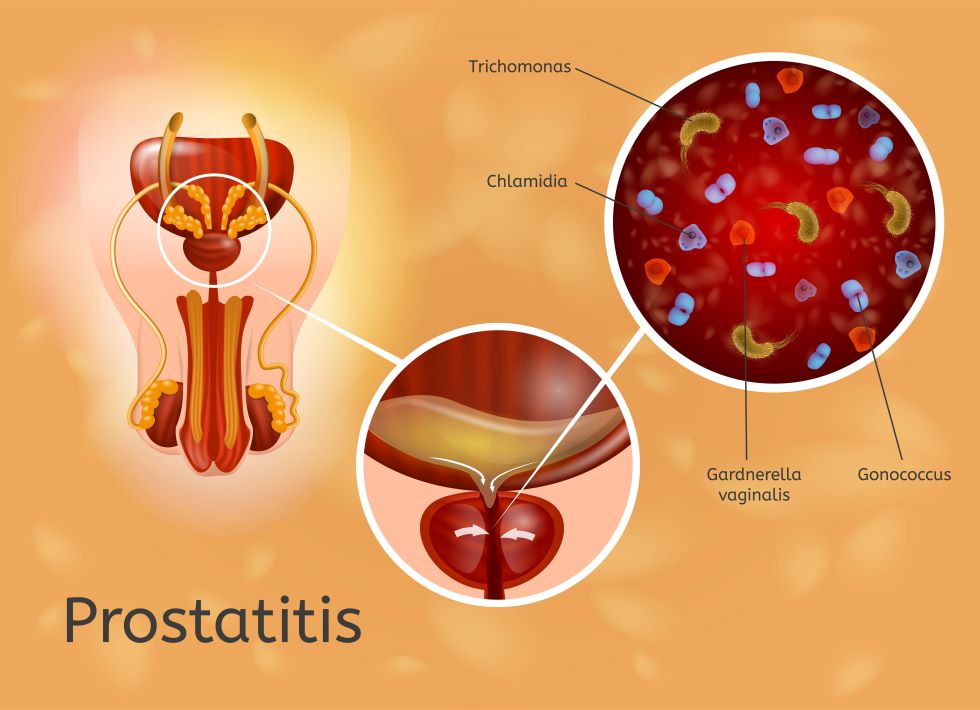
Both acute and chronic bacterial prostatitis are caused by bacteria. The bacteria may be linked to another infection, such as a urinary tract infection (UTI) or sexually transmitted infection (STI). It might also develop after a urologic procedure, such as catheterization, a biopsy, or surgery.
Bacteria can reach the prostate via the urethra or the bladder. The most common types of prostatitis-causing bacteria are Escherichia coli (E. coli), Proteus species, or staph bacteria. Bacteria from sexually transmitted infections like gonorrhea and chlamydia can also cause bacterial prostatitis.
What is the difference between acute and chronic bacterial prostatitis?
The main difference between the 2 types of bacterial prostatitis is timing.
In medical terms, acute refers to an illness that starts suddenly, could be severe, and resolves relatively quickly. In contrast, a chronic illness develops over time and takes longer to go away.
What are the symptoms of bacterial prostatitis?
Acute and bacterial prostatitis have many symptoms in common:
- urinating more frequently
- urinating more urgently
- pain or discomfort during urination
- trouble starting urination
- weak urine stream
- cloudy urine
- urinary retention (being unable to empty the bladder)
- urinary blockage (being unable to urinate)
- nocturia (having to get up during the night to urinate, interrupting sleep)
- pain in the genitals or lower abdomen
- fatigue
Men with acute bacterial prostatitis are more likely to have these symptoms:
Bacterial prostatitis might cause painful ejaculation
- fever and chills
- nausea and vomiting
- body aches
Men with chronic bacterial prostatitis might experience painful ejaculation.
It’s also possible for men with chronic bacterial prostatitis to have no symptoms at all.
Note: Men whose symptoms start suddenly and worsen quickly should see a doctor immediately. Untreated prostatitis can lead to more serious infections, prostatic abscess, and inflammation of the epididymis (the area where sperm cells are stored).
How is bacterial prostatitis diagnosed?
There are several steps involved when diagnosing bacterial prostatitis:
- Medical history. A doctor will ask questions about symptoms, urologic history, and general health.
- Urinalysis. A urinalysis is a urine test. A urine sample will be checked for bacteria and any other substances that could be linked to symptoms.
- Digital rectal exam (DRE). Digital in this case refers to digits—another word for fingers. During a DRE, a doctor will gently place a gloved, lubricated finger into the rectum. This process allows them to check the prostate for any physical abnormalities.
- Urine culture. A urine culture is another way to test for bacteria and other germs. In this case, the urine sample is placed in a petri dish in a lab. After a few days, a specialist will check the dish and analyze the contents, seeing if any bacteria or other organisms have grown or multiplied.
- Other tests. Blood, semen, and imaging tests can help doctors rule out other conditions.
How is bacterial prostatitis treated?
Bacterial prostatitis is usually treated with antibiotics. The type of medicine prescribed will depend on the type of bacteria causing the infection.
Most men need to take antibiotics for 2 to 8 weeks. Doctors may prescribe a longer course if they think the infection might return.
Men with severe cases of acute bacterial prostatitis may spend a short time in the hospital. In that setting, they will receive IV (intravenous) antibiotics and fluids. After hospitalization, a man usually needs to take oral (by mouth) antibiotics for up to 4 weeks.
What are the complications of bacterial prostatitis?
If not treated properly, bacterial prostatitis may lead to bacterial infections in other areas, such as the blood and the epididymis (the coiled tube in back of the testicle). Men may also develop chronic back pain or prostatic abscesses.
Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) affects about 2 percent to 10 percent of adult men worldwide.
What are the symptoms of CP/CPPS?
Men with CP/CPPS often report the following symptoms:
- Pain in the pelvic area, groin, or genitals. This pain may be sharp or dull, constant or intermittent. For a CP/CPPS diagnosis, the pain must last for at least 3 of the previous 6 months and not be explained by another cause.
- Urinary symptoms. Like bacterial prostatitis, CP/CPPS can have urinary symptoms, too. Men may need to urinate more frequently or urgently. They might experience pain while they urinate.
- Sexual symptoms. Some men have difficulty ejaculating or experience pain when they do so.
The severity of CP/CPPS symptoms can vary. Some men go back and forth between flare-ups and times when they’re feeling better.
Men with CP/CPPS don’t usually have a fever.
What causes CP/CPPS?
The exact cause of CP/CPPS isn’t known, but scientists are investigating. Some theories include trauma-related inflammation and autoimmune responses. (Autoimmune pertains to conditions where the body’s immune system attacks healthy tissue.)
Some experts believe psychological stress could be involved with CP/CPPS. Many men find that their symptoms worsen during times of stress.
How is CP/CPPS diagnosed?
There is no one definitive test that can diagnose CP/CPPS. Instead, doctors rule out other health conditions that can have similar symptoms, such as urinary tract infections.
Tests used to assess CP/CPPS symptoms are similar to those used to diagnose bacterial prostatitis, described above:
- Medical history, assessment of symptoms
- Digital rectal exam (DRE)
- Urinalysis
- Urine culture
- Other tests (such as blood, semen, or imaging tests)
How is CP/CPPS treated?
Men with CP/CPPS have several treatment options. Sometimes, a combination of treatments is used:
- Medications. Different medicines can target different CP/CPPS symptoms.
- Alpha-blockers (example: tamsulosin) help relax muscles near the prostate.
- Anti-inflammatories (examples: aspirin, ibuprofen) can reduce inflammation and relieve pain.
- 5-alpha-reductase inhibitors might be prescribed to men who have trouble urinating. However, these drugs might not be the best choice with men concerned about fertility, as they can affect semen volume.
- Antibiotics aren’t typically prescribed for CP/CPPS because it is not caused by bacteria. However, these drugs do help some men, especially if they have a related bacterial infection.
- Pelvic floor physical therapy. The pelvic floor is a group of muscles that hold the pelvic organs, such as the bladder, in place. Working with a pelvic floor physical therapist can reduce pain and might improve sexual function. Techniques may include Kegel exercises, relaxation therapies, biofeedback, cooling and warming, and stretching muscles and soft tissues (myofascial release).
- Cognitive behavioral therapy (CBT). Because stress can worsen CP/CPPS symptoms, some men benefit from a psychological approach called cognitive behavioral therapy. A qualified therapist can suggest ways to cope with CP/CPPS and better manage stress, depression, and anxiety.
- Acupuncture. Acupuncture is a form of traditional Chinese medicine that uses tiny needles placed through the skin. Some men with CP/CPPS find that acupuncture relieves pain.
Taking Care at Home
During treatment for bacterial prostatitis or CP/CPPS, these steps may ease symptoms:
- Avoid foods and drinks that irritate the bladder. These may include spicy foods, alcohol, caffeinated drinks (like coffee, tea, and soda), and acidic foods (like citrus fruits – oranges, grapefruits, etc.).

- Drink more liquids. Urinating more frequently flushes bacteria out of the body.
- Take warm baths (sitz baths).
- Use a heating pad or a hot water bottle.
- Try to relax and take it easy. A doctor might recommend relaxation exercises.
Resources
BJU International
Rees, Jon, et al.
“Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline”
(First published: February 24, 2015)
https://bjui-journals.onlinelibrary.wiley.com/doi/full/10.1111/bju.13101
FamilyDoctor.org (American Academy of Family Physicians)
“Prostatitis”
(Last updated: April 24, 2020)
https://familydoctor.org/condition/prostatitis/
Mayo Clinic
“Prostatitis”
(February 19, 2022)
https://www.mayoclinic.org/diseases-conditions/prostatitis/symptoms-causes/syc-20355766
Medical News Today
Newman, Tim
“What is the prostate gland?”
(Updated: November 15, 2021)
https://www.medicalnewstoday.com/articles/319859
National Institute of Diabetes and Digestive and Kidney Diseases
“Prostatitis: Inflammation of the Prostate”
(Last reviewed: July 2014)
https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostatitis-inflammation-prostate
Prostate Cancer and Prostatic Diseases
Polackwich, A. S. and D. A. Shoskes
“Chronic prostatitis/chronic pelvic pain syndrome: a review of evaluation and therapy”
(Published: March 8, 2016)
https://www.nature.com/articles/pcan20168
UpToDate
Meyrier, Alain MD and Thomas Fekete, MD
“Acute bacterial prostatitis”
(Topic last updated: October 25, 2021)
https://www.uptodate.com/contents/acute-bacterial-prostatitis
Meyrier, Alain MD and Thomas Fekete, MD
“Chronic bacterial prostatitis”
(Topic last updated: October 16, 2020)
https://www.uptodate.com/contents/chronic-bacterial-prostatitis
“Patient education: Bacterial prostatitis (The Basics)”
(Topic retrieved: January 8, 2022)
https://www.uptodate.com/contents/bacterial-prostatitis-the-basics
“Patient education: Chronic prostatitis and chronic pelvic pain syndrome (The Basics)”
(Topic retrieved: January 8, 2022)
https://www.uptodate.com/contents/chronic-prostatitis-and-chronic-pelvic-pain-syndrome-the-basics
Pontari, Michel, MD
“Chronic prostatitis and chronic pelvic pain syndrome”
(Topic last updated: September 10, 2021)
https://www.uptodate.com/contents/chronic-prostatitis-and-chronic-pelvic-pain-syndrome
Urology Care Foundation
“What is a Urine Culture Sample?”
https://www.urologyhealth.org/urology-a-z/u/urine-culture-sample
“What You Need to Know About Prostatitis”
(August 28, 2019)
https://www.urologyhealth.org/healthy-living/care-blog/2019/what-you-need-to-know-about-prostatitis
WebMD
“What’s a Urine Culture?”
(Medically reviewed: November 30, 2021)
https://www.webmd.com/a-to-z-guides/what-is-urine-culture